Breast Reconstruction
Or call us at (480) 223-9500
What is breast reconstruction?
Breast reconstruction offers women the opportunity to feel whole again after having treated breast cancer with a lumpectomy or mastectomy, or after injury or a birth defect. Most techniques involve several separate procedures that can begin as early as the time of mastectomy. Reconstruction aims to restore the shape, size, and appearance of the breast. There are several techniques by which this can be accomplished. Reconstructive options include expanding the remaining tissues on the chest and using an implant, or by using your own tissues, often taken from the abdomen or back. In addition to restoring the breast mound, there are also techniques to reconstruct the nipple and areola, including local skin rearrangements, skin grafts, and tattoos. In some cases, the remaining breast will need to be lifted, augmented, or reduced in order to improve symmetry. Please note, not all patients are candidates for every technique. Dr. Forsberg or Dr. Kelly will review the methods of reconstruction available to you during your consultation.
Although reconstructive surgery has improved with modern implants and techniques, a reconstructed breast will never have the exact same look and sensation as the breast it replaced. In addition to being prepared for the emotional adjustment involved in breast reconstruction, patients must have realistic expectations about outcomes.

Before and after breast reconstruction procedures
When and where is breast reconstruction performed?
Breast reconstruction procedures can be performed in an inpatient or outpatient setting. In most cases, a general anesthetic or a deep sedative, along with local anesthetics, are employed to ensure your comfort and safety. The initial procedures for breast reconstruction may be performed at the same time as your mastectomy, or in a delayed fashion. Immediate reconstruction offers the psychological and aesthetic advantage of waking from the mastectomy procedure with a less traumatized breast region.
What are the different types of breast reconstruction?
The two broad categories of breast reconstruction are implant-based reconstruction and autologous reconstruction – where your own tissues are used to reconstruct the breast mound. Most often, implant reconstruction begins with the placement of a tissue expander to enlarge the tissues on the chest wall slowly over a period of a few months until a permanent saline or silicone implant can be inserted in a secondary procedure. In some cases, it is possible to place a small permanent implant in the first procedure.
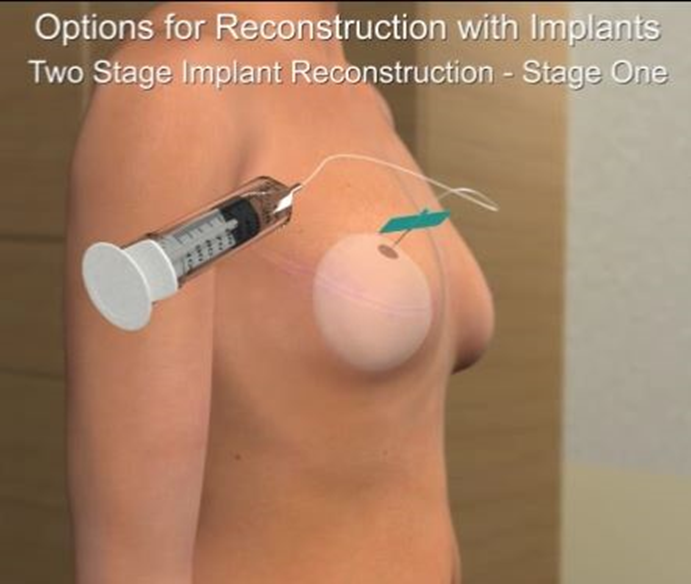
Fluid is placed into a tissue expander during an office follow-up procedure
During implant-based reconstruction, the Acellular Dermal Matrix, which is derived from human or animal tissue, may be used. Use of this product facilitates the placement of a permanent implant at the time of mastectomy. It can also be used with a tissue expander to speed the expansion process and improve the aesthetic outcome of the reconstruction. Some studies indicate these potential advantages may come at the cost of a slightly higher complication rate. You should tell your surgeon if you are opposed to the use of this product.
Autologous tissue – called a flap – from another part of your body is used to reconstruct the breast mound when a breast implant is not used. The tissue is most often taken from the abdomen or the back. Other donor options include the buttocks or thighs. Flaps can be kept attached to their dominant blood supply and tunneled into position in the chest or they can be disconnected from their native blood supply and attached to other vessels in the chest. The latter involves more operative time and a higher risk of total loss of the flap, but it can afford more versatility in the donor location or configuration of the flap. When the flap is taken from the abdomen, it will often require repair of the abdominal wall with a synthetic, mesh-like material. In general, autologous reconstructions tend to produce a more natural looking breast mound that ages with the patient and may not require as many secondary operations as implant reconstructions. It does, however, involve more operative time, longer recovery, and subjects other areas of the body to surgery.
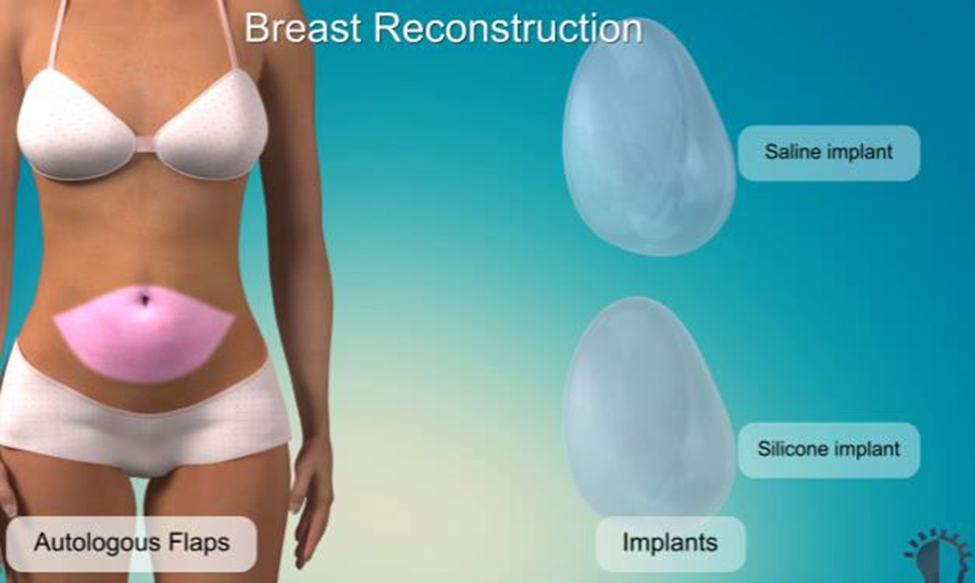
Breast reconstruction using prosthetic implants or flaps of tissue from the patient’s own body
How is the nipple reconstructed during breast reconstruction?
Nipple sparing mastectomy, where the nipple and areola are left intact while the remainder of the breast glandular tissue is removed, is becoming more widely used in some patients who are appropriate candidates. In this case, the patient’s own nipple and areola remain, and no reconstruction is necessary.
In cases where the nipple and areola are removed during mastectomy, they can be reconstructed after the breast mound is made using combinations of small tissue flaps to create an elevated nipple mound and a tatoo to create the coloration of the areola.
Is there anything else I should know?
The manufacturers of breast implants expect them to last a long time, but everything man-made does break or wear down eventually. The life span of all types of implants can be shortened by trauma or mechanical failures. A rupture, for example, may be clinically undetectable to you or your surgeon if you have silicone gel implants, but it could be picked up during mammography or other specialized tests. The rupture of the older gel implants often led to gel migration or the formation of lumps within the breast as a result of scar tissue developing around the free silicone, necessitating future breast biopsies and implant replacement. However, today’s gel-filled implants are made of a cohesive gel that stays intact even in the event of a shell rupture. They are also less likely to migrate and are easier to remove. The rupture of a saline-filled implant, on the other hand, will be obvious because the breast will return to its previous size and shape over a short period of time. Unfortunately, no one can predict in advance when an individual implant will fail. Replacing an implant will become necessary if a leak is detected. It is strongly recommended that you see your plastic surgeon at least once a year for a breast examination.
From cosmetic enhancements to medical dermatology, Center for Dermatology and Plastic Surgery is here to support you every step of the way.

